Research experts use induced pluripotent stem cells (iPSCs) to treat heart disease
Research experts use induced pluripotent stem cells (iPSCs) to treat heart disease

Copyright © iCell Bioscience Inc, Shanghai 2018-2019
On May 29th, in a journal entitled "Reprogrammed's stem cells approved to mend human hearts for the first time," published in the journal Nature, for the first time, Japanese scientists were approved by the Ministry of Health and will use induction. Pluripotent stem cells (iPSCs) treat heart disease. This is the second clinical application of iPSCs following macular degeneration.
Induced pluripotent stem cells (iPSCs) are cell types similar to embryonic stem cells (ESCs) developed by the team of scientists from the Kyoto University in Kyoto, Japan. Since its inception in 2006, induced pluripotent stem cells have been considered as a new force in regenerative medicine that can avoid the ethical concerns of embryonic stem cells and reduce the risk of immune rejection.
In 2014, the team of Masayo Takahashi, a stem cell clinical researcher at the Japanese Institute of Physical Chemistry (RIKEN), successfully used autologous induced pluripotent stem cells to treat age-related macular degeneration (a type of eye disease). However, due to safety issues, the trial was suspended after the completion of the first case.
In 2017, the RIKEN Institute reinvented itself to launch a clinical trial based on allogeneic iPSCs for the treatment of macular degeneration.
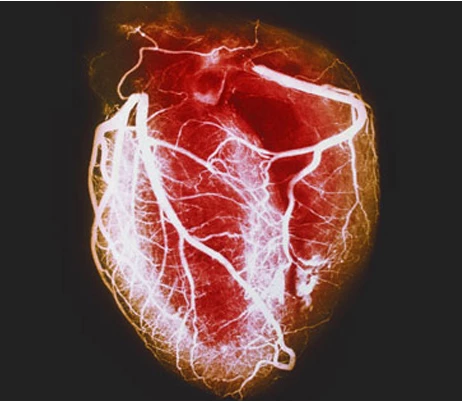
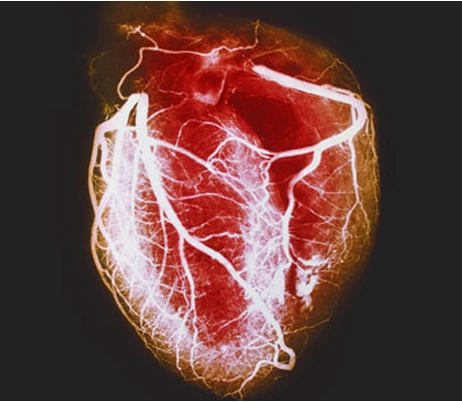
Now Yoshiki Sawa, a cardiac surgeon at Osaka University, has accumulated 15 years of research and plans to use this revolutionary cell reprogramming technology to treat heart disease. On May 16th, the Japanese Ministry of Health opened a "green light" to approve the transplantation of thin tissue from iPSCs to the damaged heart.
The team used induced pluripotent stem cells to construct a sheet containing 100 million cardiomyocytes. In a previous study, the researchers transplanted this thin slice of cells (thickness 0.1 mm, length 4 cm) onto the pig's heart and confirmed that these pluripotent stem cells can improve the function of the heart.
However, these exogenous cells do not seem to be integrated into the original heart tissue. Instead, they release growth factors that promote the regeneration of damaged myocardium.
The team believes that one of the advantages of cell sheets is the ability to construct their own cell matrix and maintain their structure so that no additional stents are needed.
It is reported that the approved clinical trials will be launched in 2019 and it is expected that 3 patients will receive treatment. After that, the scale of clinical trials was expanded to 7-10 people. If proven to be safe, this therapy will enter commercial sales under the Japan Fast Medicine System for Regenerative Medicine.
This fast-track system was launched in 2014 to accelerate the availability of life-saving therapies. But critics say the system is flawed because it allows the treatment to be commercialized to the patient before it has obtained enough effective and safe data.
This exploration has enabled researchers to bypass costly large-scale clinical trials, but based on small-scale clinical trials to demonstrate the safety and efficacy of the therapy.
Research experts said that in addition to meeting safety requirements, it is also necessary to confirm the effectiveness of cell therapy, which requires more extensive clinical validation. In addition, the review process also needs to refer to randomized, controlled clinical trials, which is the gold standard for validating efficacy in medical research.
The control experiment proved to be very important for the effectiveness of the therapy. The approval of the Ministry of Health admitted that the therapy was "scientifically and ethically reasonable" and could be tested on the patient.
 Loading ....
Loading ....
